Several beneficial mechanisms are associated with intermittent exposure to hyperbaric doses of oxygen. Either alone, or more commonly in combination with other medical and surgical procedures, these mechanisms serve to enhance the healing process of treatable conditions.
HYPEROXYGENATION: provides immediate support to poorly perfused tissue in areas of compromised blood flow. The elevated pressure within the hyperbaric chamber results in a 10-15-fold increase in plasma oxygen concentration. This translates to arterial oxygen values of between 1,500 and 2000 mmHg, thereby producing a four-fold increase in the diffusing distance of oxygen from functioning capillaries.
NEOVASCULARIZATION: represents an indirect and delayed response to hyperbaric oxygen exposure. Therapeutic effects include enhanced fibroblast division, neo-formation of collagen, and capillary angiogenesis in areas of sluggish neovascularization such as late radiation damaged tissue, refractory osteomyelitis, and chronic ulcerations in soft tissue.
HYPEROXIA: enhanced ANTIMICROBIAL ACTIVITY has been demonstrated at a number of levels. Hyperbaric oxygen causes toxin inhibition and toxin inactivation in Clostridial perfringens infections (gas gangrene). Hyperoxia enhances phagocytosis and white cell oxidative killing, and has been shown to enhance amino glycoside activity. Recent research has demonstrated a prolonged post-antibiotic effect, when hyperbaric oxygen is combined with “Tobramycin” against “Pseudomonas aeroginosa”.
DIRECT PRESSURE:utilizes the concept of Boyle's Law to reduce the volume of intravascular or other free gas. For more than a century, this mechanism has formed the basis for hyperbaric oxygen therapy as the standard of care for decompression sickness and cerebral arterial gas embolism. Commonly associated with divers, Acute Gas Embolism is a frequent iatrogenic event in modern medical practice. It results in significant morbidity and mortality and remains grossly under diagnosed.
HYPEROXIA-INDUCED VASOCONSTRICTION
is another important mechanism. It occurs without component hypoxia, and is helpful in managing intermediate compartment syndrome and other acute ischemia in injured extremities, and reducing interstitial edema in grafted tissue.
ATTENUATION OF REPERFUSION INJURY:
is the most recent mechanism to be discovered. Much of the damage associated with reperfusion is brought about by the inappropriate activation of leukocytes. Following an ischemic interval, the total injury pattern is the result of two components: a direct irreversible injury component from hypoxia, and an indirect injury, which is largely mediated by the inappropriate activation of leukocytes. Hyperbaric oxygen reduces the indirect component of injury by preventing such activation. The net effect is the preservation of marginal tissues that may otherwise be lost to ischemia- re-perfusion injury.WHERE HYPERBARIC OXYGEN THERAPY HELPS : :
These are the indications approved by the American “UHMS Organization”..
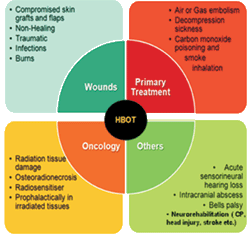
The treatment of choice for air or gas embolism of the arterial or venous system is recompression in a hyperbaric chamber. Recompression is indicated for the following types of air emboli:
- Surgical
- Diagnostic Procedures
- Renal Dialysis
- Pulmonary Over-Pressure During Scuba Diving
- Cardiovascular Surgery
When gases enter the vasculature in sufficient volume to compromise the function of an organ or body part, the process can create varying degrees of ischemia to the affected areas. Treatment is most effective when initiated within minutes of the incident. However, evidence has shown that delayed and repeat treatment has demonstrated a means to a more expedient recovery.
RATIONALE:
Recompression of gas bubbles as well as the rescue of hypoxic tissue by way of HBO2 treatment is the only form of treatment known. HBO2 reduces the mortality rate and remedies the development of permanent neurological damage.
Hyperbaric oxygen (HBO2) treatment is indicated for the following signs and symptoms in cases of CO2 inhalation:
- Alteration in Mental Status
- Neurological Signs
- Cardiovascular Dysfunction
- Pulmonary Edema
- Severe Acidosis
- Carboxyhemoglobin Levels in Excess of 25%
Patients who manifest any of the first five signs listed above should be referred for HBO2 treatment irrespective of their carboxyhemoglobin level. Treatment is most effective when initiated within six hours of exposure.
RATIONALE: HBO2 treatment must be predicted more on the clinical picture than the carboxyhemoglobin levels. HBO2 hastens the disassociation of carbon monoxide from hemoglobin, myoglobin, cytochromes and other hemoproteins.
RATIONALE: Carbon monoxide and cyanide poisoning frequently occur simultaneously in victims of smoke inhalation. These two agents in combination exhibit synergistic toxicity. HBO2 may have a direct effect in reducing the toxicity of cyanide and augmenting the benefit of antidote treatment. HBO2 increase in plasma dissolved oxygen content may offer a direct benefit.
Hyperbaric oxygen (HBO2) therapy is an adjunct to surgery and antibiotics for the treatment of clostridial myositis and myonecrosis (gas gangrene) and spreading clostridial cellulitis with systemic toxicity, or a presumptive diagnosis of either.
Treatment should be started without delay because less surgery needs to be performed and the cessation of alpha-toxin production is rapid.
RATIONALE: Ninety percent of the cases of gas gangrene are caused by the organism Clostridium perfringes. However, a number of pathogenic clostridial organisms may be involved. These organisms produce necrotizing tissue toxins. Clostridium perfringes is not a strict anaerobe; it may grow rapidly in oxygen tensions of up to 30 mmHg and in a restricted manner in oxygen up to 70 mmHg.
Hyperbaric oxygen (HBO2) treatment should begin during the acute episode. Recompression is indicated for the following clinical manifestations:
- Profound Fatigue
- Neurological Dysfunction
- Joint Pain
- Skin Eruptions
RATIONALE: The disease arises from the generation of nitrogen bubbles in the vascular system and tissues in volumes sufficient to interfere with the function of an organ or cause alterations in sensation. The cause of gas bubble formation is the rapid decompression during ascent from diving, flying or a hyperbaric chamber when the speed of decompression exceeds the ability of the gas saturated tissues to vent the gases by simple diffusion. Secondary effects of the nitrogen bubble at the blood bubble interface can include activation of the complement system, lymph phobic effects and increased blood viscosity. Prompt treatment is important to reduce bubble size and repetitive treatments may be necessary for patients with residual defects following the initial recompression.
Hyperbaric oxygen (HBO2) treatment must be initiated as soon as possible (usually within 48 hours) and must be used as an adjunct to standard surgical treatment including vascular repair as indicated.
RATIONALE: Crush injury involves severe trauma to bone, soft tissue, nerve, and vascular structures. Acute traumatic ischemia occurs when there is a severe injury to a limb and the circulation of the extremity becomes compromised. This ischemic compromise may be severe enough to place the entire extremity at risk of necrosis and amputation.The primary rationale for using HBO2 is that it increases tissue oxygen tensions to levels, which make it possible for the host responses to become functional. At 2 ATA, the blood oxygen content is increased by 25% whereas plasma and tissue oxygen tensions increase tenfold (i.e. 1000%). The net effect is that oxygen diffusion through tissue fluids is increased by a threefold factor. Sufficient oxygen becomes physically dissolved in the plasma to keep tissues alive despite inadequate haemoglobin-borne oxygen. Oedema reduction secondary to vasoconstriction is another effect of hyper oxygenation. This mechanism reduces blood flow by 20%. The benefit of vasoconstriction is a concomitant (i.e. 20%) reduction in posttraumatic vasogenic oedema. In effect, HBO2 maintains oxygen delivery while blood flow is improved in the microcirculation by the oedema reducing effect of vasoconstriction. Thus, the immediate effects of HBO2 are threefold in acute traumatic ischemia: a) enhanced oxygenation at the tissue level, b) increased oxygen delivery per unit of blood flow, and c) oedema reduction. Therapy should be initiated within 48 hours after the injury; however, to be most effective, treatment should be started within the first 4 to 6 hours.
Problem wounds are those which fail to respond to established medical/surgical management. These wounds usually present in compromised hosts with multiple local and systemic factors which inhibit tissue repair. These include:
- Diabetic Wounds
- Compromised Amputation Sites
- Nonhealing Traumatic Wounds
- Vascular Insufficiency Ulcers
RATIONALE:
Hyperbaric oxygen (HBO2) treatment provides a significant increase in tissue oxygenation in the hypoperfused, infected wound. This elevation in oxygen tension induces significant positive changes in the wound repair process. HBO2 promotes wound healing by directly enhancing fibroblast replication, collagen synthesis, and the process of neovascularisation. Providing oxygen at the cellular level also increases leukocyte bacterial activity and has a direct lethal effect on anaerobic organisms.
Hyperbaric oxygen (HBO2) therapy is not necessary nor is it recommended for the support of normal, uncompromised skin grafts or flaps. However, following preoperative or postoperative irradiation or in other cases where there is decreased microcirculation or hypoxia, HBO2 has been shown to be extremely useful in preserving these compromised grafts and flaps. HBO2 is also effective in promoting capillary proliferation and granulation to prepare a surgical site.
RATIONALE: The literature clearly shows the efficacy of HBO2 with respect to enhancement of wound healing and skin graft and flap survival. Although the blood supplies are very different in these flaps, a key factor to flap necrosis is tissue hypoxia. The results indicate that viability of flaps can be enhanced by HBO2 through a reduction of the hypoxic insult. Other mechanisms of action, whereby, enhances flap survival include the enhancement of fibroblasts and collagen synthesis, neovascularity, and the possibility of closing off arteriovenous shunts. To be maximally effective, HBO2 therapy should be started as soon as there is any doubt as to the viability of the flap.
The burn wound is a complex and dynamic pathophysiologic process characterized by a zone of coagulation, surrounded by a region of stasis, and bounded by an area of hyperaemia. An intense inflammatory reaction leading to rapid oedema formation, increased micro vascular permeability, and sluggish blood flow results in thrombosis, ischemia, and advancing necrosis. The basic problems in repair of burns include susceptibility to infection, prolonged healing, and excessive scarring. These problems are greatly increased due to the loss of the integumentary barrier to bacterial invasion and compromised or obstructed microvasculature.. Adjunctive hyperbaric oxygen (HBO2) therapy can attack these problems, directly maintaining micro vascular integrity, minimizing oedema, and providing the substrate necessary to maintain viability.
RATIONALE:
HBO2 therapy has been shown to exert a positive, beneficial effect on the burn wound by:
(1) reducing edema and plasma extravasation,
(2) preserving the microcirculation,
(3) preventing the conversion of partial to full thickness injury, and
(4) maintaining the viability of the dermal elements which lead to a more rapid epithelialization.
This has lead to a reduced need for surgery, a reduced length of hospital stay, and a reduced mortality rate. HBO2 therapy, used as an adjunct to traditional burn care, demonstrates greatest effects when initiated within the first 4 hours following the injury, or as quickly as possible.
Hyperbaric oxygen (HBO2) treatment is to be used as an adjunct to surgical and antibiotic treatment. Necrotizing mixed flora (aerobic and anaerobic) infections usually occur in traumatic or surgical wounds around foreign bodies and affect patients who are medically compromised by either diabetes mellitus, vascular insufficiency, or both.
RATIONALE: Hypoxic conditions profoundly impair polymorphonuclear (PMN) leukocyte function and as infection develops metabolism by facultative organisms further depletes the oxygen that is available. This action as well as accumulation of metabolic products improves conditions for the growth of anaerobic bacteria. Surgical debridement and systemic antibiotics are the principal treatment protocol for necrotizing soft tissue infections.
The oxygen tension in infected tissue is low. Increasing tissue oxygen tensions enhances white cell killing of bacteria, promotes inhibition of anaerobic organism growth and increases the oxidation-reduction potential.
Refractory osteomyelitis is chronic osteomyelitis that has persisted or recurred after appropriate interventions have been performed or where acute Osteomyelitis has not responded to accepted management techniques. HBO2 adjunctive therapy, aggressive surgical debridement, parenteral antibiotics (or equivalent) and nutritional support improve patient outcomes. HBO2 should be initiated immediately following surgical debridement of infected bone.
RATIONALE: HBO2 promotes angiogenesis, increased leukocyte killing, aminoglycoside transport across bacterial cell walls, and osteoclast activity in removing necrotic bone. When used according to guidelines, HBO2 is clinically efficacious and cost effective.
Radiation tissue damage includes soft tissue radio necrosis, osteoradionecrosis, radiation mucositis, dermatitis, enteritis, laryngeal radio necrosis, cystitis, etc. and surgical wounding in radiation-damaged tissues. Hyperbaric oxygen (HBO2) therapy must be part of an overall plan in which debridement, resection of nonviable tissues, bone grafting, myocutaneous flap reconstruction, and specific antibiotic therapy may be included.
RATIONALE: With daily elevation of oxygen tension in hypoxic, hypo cellular, and hypovascular bone and soft tissue near regions of functioning capillaries, fibroblast proliferation, collagen synthesis, and angiogenesis proceed. The killing ability of leukocytes is enhanced with the elevation of tissue oxygen tensions
There have been anecdotal reports of patients with cerebral abscess who have recovered following HBO2 treatment.
Exceptional blood loss (anaemia) occurs when the patients has lost sufficient red cell mass to compromise respiratory requirements and cannot or will not receive transfusions because of medical or religious reasons.
RATIONALE: The intermittent use of hyperbaric oxygen (HBO2) therapy will supply enough oxygen in the severely anaemic patient to support the basic metabolic needs of the respective tissues of the body until red blood cells are restored. Most vitally, our brain requires approximately 6 volumes percent of oxygen to support its basic metabolic requirements. HBO2 therapy at 3 ATA will place 6 volumes percent of dissolved molecular oxygen in an intravascular acellular perfusate for the direct use by tissue cells.HBO2 is discontinued when the red blood cells have been replaced in numbers so as to alleviate the above signs and symptoms (a hematocrit of approximately 23%). There is presently no satisfactory blood substitute available to use in exceptional blood loss anaemia. Thus, HBO2 is a valuable adjunct when used early in treating acute blood loss in those who cannot or will not receive blood replacement for medical or religious reasons.
Sudden Sensorineural Hearing Loss (SSNHL) is hearing impairment of more than 30 dB of three consecutive pure tone frequencies developing within 3 days or less. Due to lack of definite cause of SSNHL, its treatment is largely empirical and includes use of a wide variety of therapies like systemic and Intratympanic steroids, vasodilators, osmotic drugs, antiviral and anticoagulants to counteract possible inflammatory mechanism, modify hydrostatic pressure and improving cochlear blood flow. Hyperbaric oxygen therapy is a treatment modality involving the intermittent inhalation of 100% oxygen in chambers pressurized above 1 atmosphere absolute (ATA). HBOT has been used as an adjunctive therapy for SSNHL as it raises the amount of oxygen in the inner ear by diffusion which activates cell metabolism leading to restoration of ionic balance and electrophysiological functions of cochlea
List of “RESEARCH INDICATIONS”
Although still counted among the research indications, the role of HBOT has been proved in treatment of MI.
The American Heart Association Endorses HBOT for Heart Attack
Clinical investigations by prime users of HBO from around the world, especially from Russian exponents, has shown the following heart advantages:
- HBOT normalized electrocardiograms in all patients in that same Soviet study.
- For diminished muscular power of the heart, HBO exerts long-term normalizing effects for circulating blood through the body.
- HBOT exerts antiarrhythmic action on the heart.
- HBOT increases heart patients' tolerance to hard work and taking on physical loads.
The time from primary brain injury to the occurrence of irreversible damage varies considerably, depending upon the severity of the injury and degree of hypoxia. There is clinical and experimental evidence suggesting that hyperbaric oxygen (HBO2) treatment is beneficial in reducing mortality and improving the functional recovery of survivors.
RATIONALE: HBO2 increases the amount of oxygen dissolved in the blood, therefore decreasing the possibility of hypoxia. HBO2 causes vasoconstriction without reducing the tissue oxygen concentration. The HBO2 induced vasoconstriction also reduces swelling.
In acute and semi-acute neurologic conditions, where there is no matrix, pressurized oxygen has beneficial effects in that it not only dissolves in cerebrospinal fluid, but also:
- Reduces cerebral edema;
- Reduces intracranial pressure;
- Elevates diffusional driving force for oxygen, increasing tissue oxygen availability;
- Restores the integrity of the blood-brain barrier and cell membranes;
- Neutralizes toxic amines;
- Increases neovascularization (over time);
- Acts as a scavenger of free radicals;
- Promotes phagocytosis (thereby internal debridement);
- Stimulates angiogenesis (over time);
- Reactivates idling neurons;
- Inhibits anaerobic glycolysis;
- Promotes epithelization;
- Deglutination of platelets;
- Makes available molecular oxygen for immediate use without energy transfer;
- Reduces lactate peak in hypoxia.
Hyperbaric oxygen, if applied very early in poisoning, will significantly protect the liver from damage in carbon tetrachloride ingestion.
There have been sporadic reports in the literature, including recent ones from Australia, which tend to show that hydrogen sulfide poisoning is benefited by HBO2.
There have been anecdotal reports showing dramatic relief of sickle cell crisis with hyperbaric oxygen. Original work done at Duke University showed that sickle cell forms of the erythrocyte were markedly reduced under hyperbaric conditions.
HBOT can prevent permanent injury in non-transecting lesions of the spinal cord when applied within four hours of injury. However, in the clinical setting, it is typically very difficult to get the patient to a chamber within four hours of injury.
This often-fatal disease, which appears secondary to pneumococcal pneumonia and meningococcemia, has been shown to respond to hyperbaric oxygen. The disease is most common in children, and fingers, toes and even limbs may be lost to peripheral ischemia.
Normally this is a surgical disease where one operates to remove dead bowel. However, often too much bowel appears to be infarcted to be compatible with survival. Some of these patients were subsequently treated for three days in a hyperbaric chamber and appeared to have more viable bowel after treatment. Operation then became possible.
A large series of occluded central retinal arteries have been reported from Japan (Miyake, 1986). Approximately 50% of these patients will respond to hyperbaric treatment. This treatment is experimental but it is advantageous to try it as there is little other to offer these patients. Patients who have a totally dead retina, evidenced by being unable to tell the difference between light and dark, do not respond to hyperbaric oxygen.
This is a disease of the eye found in patients who have had their lenses removed for cataract with placement of a plastic replacement lens. A study was done in Denver (Pfoff & Thom, 1986). It was found that the first five patients had 100% success in clearing up their vision. One patient improved from 20/400 to 20/40. Results seemed to be permanent in that the treatment was stopped after three weeks and the eyes remained stable for 1-1/2 years.
This is an idiopathic paralysis of the face which typically occurs in young adults. Most cases will clear spontaneously in six months. However, some patients never completely recover. Steroids are the only treatment currently used and results are inconclusive as to their benefit. (The Undersea and Hyperbaric Medical Society published a larger study of 79 patients, completed by Racic, et al, in 1997).
The Mycobacterium leprae is sensitive to high partial pressures of oxygen. There have been reports in the literature that six treatments carried out over a three-day period have produced permanent remission (Wilkinson, et al, 1969)
Hyperbaric oxygen (HBO2) is thought to exhibit its effects through enhanced tissue oxygenation and possible inactivating effects on Loxosceles venom, however this remains to be proven.
Lyme disease is a bacterial infection caused by a spirochete, Borrelia burgdorferi (Bb), and believed to be microaerophilic. The study suggests that the Bb organism is sensitive to elevated levels of oxygen at elevated tissue partial pressure above 160 mmHg and this can be achieved by HBO2 therapy. The results of the study show improvement in approximately 85% of those treated through a decrease or elimination of symptoms.













.png)